On Dec. 31 of last year, Chinese authorities alerted the World Health Organization to a mysterious virus causing pneumonia-like illness in a small cluster of patients in the city of Wuhan. Shortly after, the novel virus was identified as SARS-CoV-2. It has since escalated into a global pandemic with outbreaks on six continents, causing disruption to our lives at a scale never seen in this lifetime.
Just a few months ago, the scientific community didn’t know this virus existed. And now, understanding SARS-CoV-2 and the disease it causes — COVID-19 — will be critical to developing treatments and helping to stop it from spreading further.
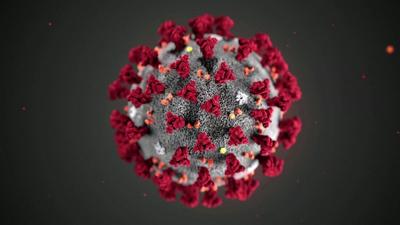
Coronaviruses are a large family of viruses named for the crown-like protein spikes on their outer surface. There are seven well-described coronaviruses that infect humans, causing respiratory illnesses that range from the common cold to more severe illnesses such as Severe Acute Respiratory Syndrome (SARS), Middle Eastern Respiratory Syndrome (MERS) and most recently, COVID-19.
Read on to learn more about the basic science of coronaviruses and SARS-CoV-2.
They have the largest RNA genome among viruses.
Coronaviruses consist of a single strand of RNA bound by protein and wrapped in an “envelope” of lipid molecules. Among known viruses that use RNA (instead of DNA) as their genetic material, they have the largest continuous genome, about 30,000 nucleotides long. With a longer genome, there is more opportunity for mutations during replication. “Viruses with large RNA genomes typically have mechanisms that help them to survive despite having lots of individual members of the virus population with deleterious errors in their genomes,” says Phil Dormitzer, Vice President and Chief Scientific Officer for Viral Vaccines based at Pfizer’s Pearl River, New York, research site. But higher rates of mutation also allow more chances for the virus to develop new characteristics, such as the ability to infect a new cell type or a new species.
Another key to their survival: Coronaviruses have high rates of natural recombination, which occurs when more than one coronavirus strain infects the same cell, and they swap genes during replication, creating a new viral strain. Recent genomic analysis reveals that COVID-19 may have resulted from recombination between two different existing viruses. “It is possible that a natural recombination event between coronaviruses contributed to this generation of SARS-CoV-2,” says Dormitzer.
The virus uses its outer “spike” proteins to bind to human cell receptors.
In the first step in infection, the novel coronavirus, or SARS-CoV-2, uses its spike protein to bind to a receptor called ACE2 found in the cells of the lung and other organs. It then fuses its oily membrane with the membrane of the host cell and releases its genetic material. Once the virus has overtaken the cell, it hijacks the cell’s internal machinery to make proteins that help it replicate.
It is possible that a natural recombination event between coronaviruses contributed to this generation of SARS-CoV-2.
All coronaviruses use these outer spike proteins to invade cells. But these proteins have different surfaces depending on the specific strain. One of the keys to developing a vaccine will be to match the spike antigen in the vaccine to the spikes on circulating coronavirus strains.
SARS-CoV-2 may have originated in bats and hopped into an “intermediate” species before being able to infect humans.
Many viruses are species specific — they are equipped with a set of characteristics to attach to the right receptors in their host and then enter cells and replicate. But a variety of genetic changes can result in a virus crossing over into another species.
There are hundreds of coronaviruses that infect bats, making them the source for many coronaviruses that infect other animals, says Dormitzer. The 2002-2004 SARS epidemic traces its origins back to bats, but passed through an intermediary species, a palm civet (a cat-like creature) or racoon dog, before infecting humans. Scientists have found that the novel coronavirus has genetic similarities to a bat coronavirus and to a pangolin coronavirus. “Although the story is not yet fully worked out, a similar evolutionary path starting in bats and progressing through an intermediate species, like the pangolin, seems likely,” says Dormitzer.
Several factors will determine the future course of the novel coronavirus.
Scientists are still unsure of how seasonality will factor into the virus’s survival. For influenza, it’s been shown in the lab that humidity affects levels of transmission, with drier air being more favorable for spreading. But the novel coronavirus is too new a human pathogen to have been studied thoroughly.
With testing for the virus currently limited, scientists don’t have a true picture of its rate of infection. Researchers need to measure how many people may have been exposed to the virus, regardless if they’ve been ill, to better understand how much the virus has circulated. “If many people have been infected for each of the cases of illness that we are observing now, herd immunity will build up more quickly, curtailing virus spread. If only a few people are infected for every case of illness, we’ll have further to go before herd immunity starts to slow the spread,” says Dormitzer.
Finally, scientists also need to understand how long immunity lasts. “If immunity is lifelong, once all adults and older children have been either infected or immunized, COVID-19 could become a childhood disease and, fortunately, severity appears to be generally mild in young children. If immunity is not durable, recurrent outbreaks of severe disease in older adults are more likely.”
